Dr. Luis Montaner, Wistar’s Associate Director for Shared Resources, and Mark Drinker, Wistar’s Associate Director for Administration of the Ellen and Ronald Caplan Cancer Center, chat about core facilities that support the innovations of our Wistar scientists, particularly spotlighting Wistar’s new Humanized Models of Disease Core.
Q: Can you tell our readers why it is so important that Wistar has Shared Resources? We’re a small biomedical research institute, why do we need it?
Mark: Wistar Shared Resources are mission critical. Every institution needs to have core facilities that support and are tailored to the science taking place in their organizations or institutes. Shared Resources allow faculty to incorporate leading-edge technology into their science in order to advance their research programs. Shared Resources may be created as a result of technology developed within an individual laboratory. For example, a laboratory may develop technology and expertise that is critical to advance their own science, and over time many other labs find they have that same need. This could be the impetus of the technology to be scaled into a Shared Resource designed to meet the needs of many researchers.
Q: Can you explain your work as the Associate Director for Administration of the Ellen and Ronald Caplan Cancer Center Shared Resources?
Mark: I work closely with Dr. Montaner, our Shared Resources director, and our Cancer Center leadership to position our core facilities as research engines that serve as extensions of our faculty laboratories. The goal is to maintain state-of-the-art Shared Resources that advance the research efforts of Wistar faculty and research partners. To accomplish this, our Shared Resources all contain technology, high-tech equipment, and exceptional personnel who have the expertise to work with each individual laboratory at Wistar.
Q: Can you describe some of the goals of the new Humanized Models of Disease Core, as its Scientific Director?
Luis: With the new Core under Dr. Zhe Yuan as Managing Director, we hope to generate a resource of humanized mice that could be of service to infectious disease scientists within the Vaccine and Immunotherapy Center, as well as the Cancer Center faculty. This model allows researchers to study how tumors from persons grow or respond to therapy if implanted in mice as well as how the human immune cells interact with tumors. The core is an investment to generate enough expertise in-house so we can bring a humanized mouse (differentiated with the human immune system) to the laboratory. The core will allow Wistar teams to utilize the humanized mouse as needed to move their experiments forward.
Q: What are humanized models of disease and why are they important?
Luis: A humanized model of disease is utilizing an animal model to study human physiology. The ability to study human immune cells within tissue enviroments for long periods of time (weeks) provides for studies that may better resemble our human body. We can use these models to study the infectious disease process of pathogens that infect human blood cells such as HIV. We can also use it for understanding human tumors.
Q: What was the impetus behind creating the Humanized Models of Disease Core Facility?
Mark: For many years Wistar faculty, including Drs. Herlyn and Montaner, have been developing mouse models to study cancer and infectious disease. Our scientists need to utilize models that closely replicate the human immune system to test their hypotheses. By creating a Shared Resource, we hope to develop a structure that allows Wistar to maintain this promising technology and offer it broadly to our research teams in order to advance their science.
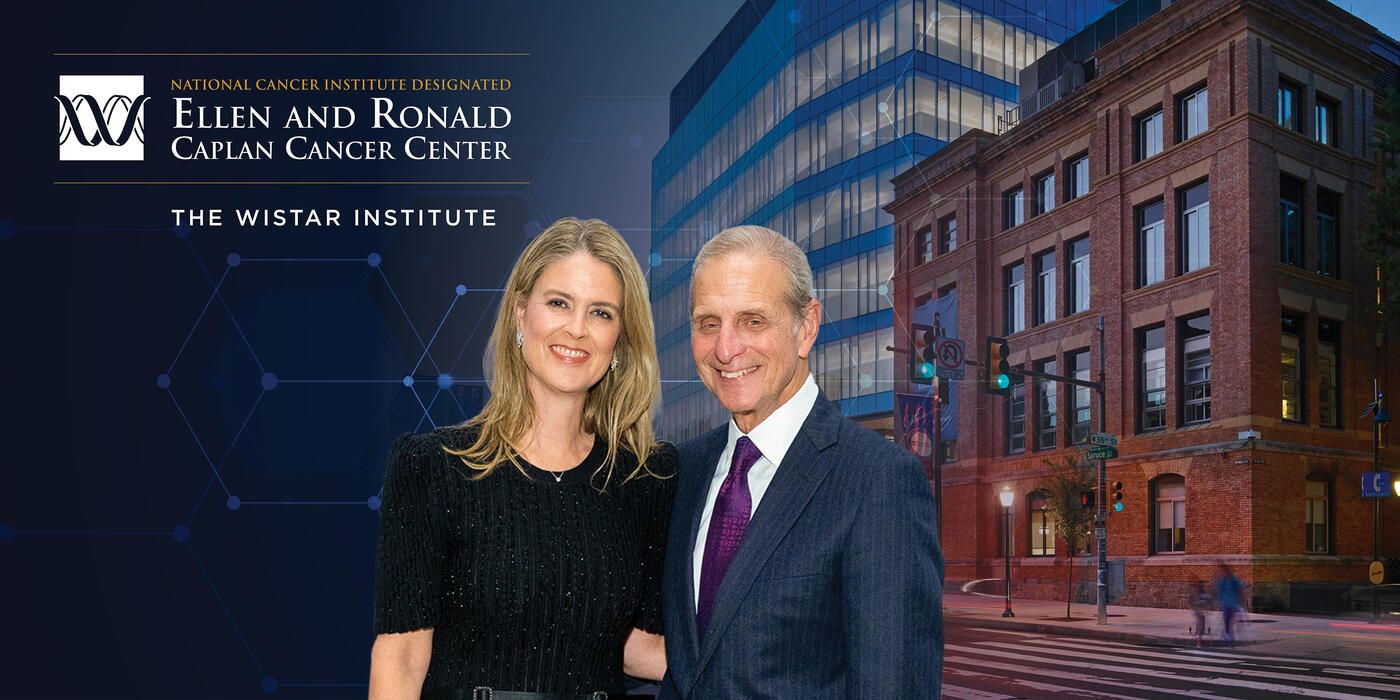
Luis: Innovative science is made possible by the strong support of our donors. This new facility is just one example of the progress Wistar can accomplish with the generosity from our philanthropic community. The ability to propel research forward is facilitated by those who believe Wistar science is an impactful investment for the future. The creation of the new center is supported by a philanthropic commitment to Wistar’s most important priorities, which is to advance our technologies and scientific resources available to our researchers. The discoveries that will be made are the fruits of investing philanthropically in The Wistar Institute.
Q: Can you give me some examples of the scientific information that can be collected from using these models?
Luis: To study novel therapeutic strategies, you can use a tissue culture plate that just has the cells that you want to interact or understand. But once you start reconstituting the way our bodies are, then you must start scaling up into systems too. How well can I reach the blood with this drug that is in circulation to maintain this change? How well can I add a drug that would reach the cells in a physiological state? If it’s an organ system, how well can I get to that organ for my treatment to still work in the microenvironment of the lung, or the liver, or the gut? As we look for what model systems do, we must start scaling into a whole system.
When it comes to generating a platform to pilot test some proof of principle or evidence that this treatment could work in the context of human cell interactions, the humanized mice model becomes one tool that is a lot less costly and a lot less demanding with respect to using limited resources. The use of the humanized mouse model becomes a tool that could potentially give a researcher more confidence that what they’re working on is worth advancing.
Q: Can you describe some of your own HIV research and how it could be impacted by this new facility?
Luis: The humanized mouse model gives you the ability to screen many ideas within a model. Underway in our BEAT-HIV Martin Delaney Collaboratory efforts at Wistar, we are developing and testing novel strategies of viral eradication by 1) activating the immune system to clear HIV-infected cells, and 2) directly targeting HIV by CRISPR CAS9 and other gene editing approaches to rid the viral infection directly from the cells. This model gives us the ability to screen multiple strategies that either target infected cells directly or target the immune system to clear infected cells due to the immunotherapy.
Q: What do you hope that researchers will get out of using this facility?
Luis: As the technology keeps moving forward, the application of humanized mouse models in cancer research are starting to become a higher priority. For example, we can place patient tumors into mice that have compatible immune systems matched with the tumor. It’s also going to be important to test immunotherapies or chemotherapies in the context of cancer eradication as well as for the infectious disease research of the Vaccine and Immunotherapy Center.
We all have a particular signature to our immune systems, and the best model is to generate a mouse that has the same signature of the person that the tumor has been growing in (i.e., creating a personalized research model). Studying therapy approaches where a tumor also matches the immune system of the person in the same mouse allows us to identify personalized cancer therapies. These types of models are now becoming more possible.