A decade-long collaboration between Wistar and ChristianaCare is leading to new discoveries and better treatment for triple-negative breast cancer patients.
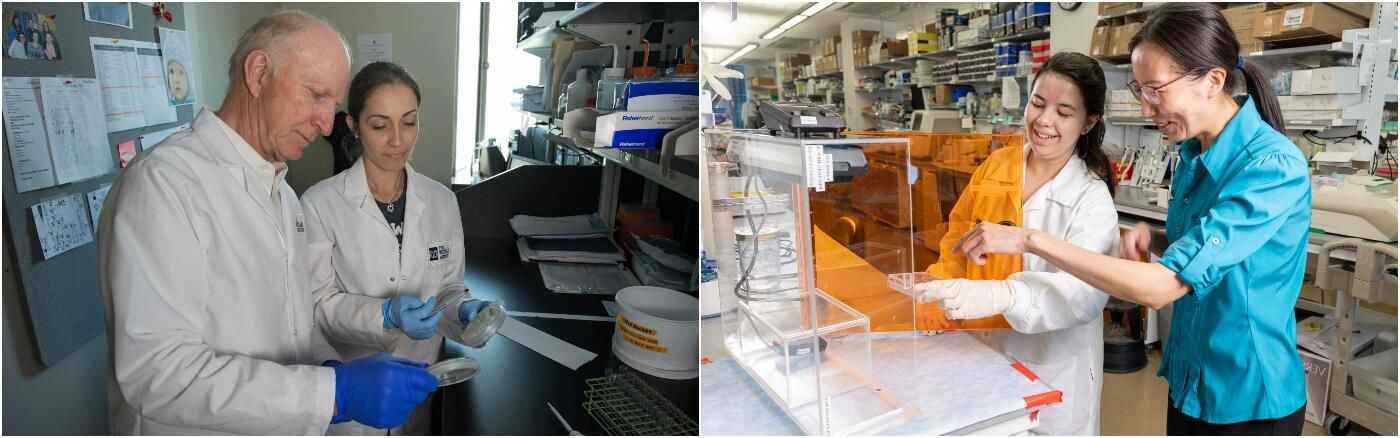
Dario C. Altieri, M.D., president, CEO, and director of the Ellen and Ronald Caplan Cancer Center at The Wistar Institute, and Nicholas J. Petrelli, M.D., Bank of America endowed medical director of the Helen F. Graham Cancer Center & Research Institute at ChristianaCare, formed a collaboration between the two institutions that would expedite the pipeline of cancer interventions from bench to bedside.
“We had the patients, and they had the world-class science,” said Petrelli. “We felt that this was a great opportunity between an NCI-designated, basic science research center and an NCI community cancer center. This relationship is unique in cancer research.”
This collaboration has yielded more than a dozen translational cancer research papers to date and advanced research discoveries made in Wistar labs into early clinical trials at ChristianaCare. One of the newest projects to come from this collaboration is a population health study on treating triple-negative breast cancer.
RESEARCHING TRIPLE-NEGATIVE BREAST CANCER
Triple-negative breast cancer is an aggressive form of breast cancer with few treatment options. It’s more than twice as common in Black women as in white women, and Black women have a 40% higher mortality rate [1, 2]. These factors are what led Zachary Schug, Ph.D., an assistant professor in the Molecular and Cellular Oncogenesis Program at Wistar’s Ellen and Ronald Caplan Cancer Center; Jennifer Sims-Mourtada, Ph.D., lead scientist and director of Translational Breast Cancer Research at ChristianaCare’s Helen F. Graham Center & Research Institute; and Scott Siegel, Ph.D., MHCDS, director of population health research at ChristianaCare to join forces.
Siegel says, “Disparities in breast cancer are the result of multiple interacting factors operating at different scales, so if we’re going to do something meaningful, we can’t take a silo-based approach and focus on one key variable. We really do need to look across this spectrum.”
ALCOHOL AND BREAST CANCER
Schug, Sims-Mourtada, and Siegel share three intersecting research interests: breast cancer, health disparities, and investigating the connection between alcohol and cancer – truly the linking factor in the context of this project.
As a molecular and cellular biologist, Schug examines the problem of alcohol and breast cancer at the “smallest” level of the three researchers. His research has shown that breast tumors feed on a breakdown product of alcohol called acetate, which they use to grow and fight the body’s immune responses. How and why the breast cancer cells use acetate in this way are questions Schug continues to pursue. However, it’s important for him to make his work clinically meaningful as quickly as possible.
“Instead of just focusing on individual tumor cells and trying to do things at a
molecular level, we wanted to ask more broad questions,” Schug explains, “and
that’s where Scott and Jen come in with what they’re doing.”
GENETICS AND ALCOHOL METABOLISM
Sims-Mourtada is a translational breast cancer researcher who studies how gene expression regulates and alters the progression of breast cancer. Her work intersects neatly with Schug’s because she is investigating whether race-based differences at the genetic level affect how many alcohol-metabolizing enzymes are produced in breast cancer stem cells.
“We have some data that show that a certain isoform of enzyme is overexpressed in tumors from Black women, and a possible reason for this could be some kind of genetic factor,” said Sims-Mourtada. Specifically, there are reports from alcohol use disorder research suggesting the existence of tiny genetic variations called single nucleotide polymorphisms (SNPs) that may be involved in alcohol metabolism. Sims-Mourtada is working on identifying SNPs that might cause an alcohol-metabolizing gene to become overactive or underactive in individuals of differing races which, combined with the individual’s alcohol use, could increase tumor growth.
ALCOHOL-RELATED ENVIRONMENTS AND BEHAVIORS
Siegel looks at the problem of triple-negative breast cancer at a population level. His research focuses on identifying modifiable risk factors for cancer—i.e., whether people’s cancers can be affected by where they live and what they do.
“My contribution to this project is to collect behavioral data on patients. Then we can relate these variables to the processes Jennifer and Zach are looking at, including the enzymes that metabolize alcohol and ultimately the metabolites,” said Siegel.
In examining prevalence of triple-negative breast cancer within ChristianaCare’s home state of Delaware, he found that the areas that have the highest rates of this cancer also have the highest rates of alcohol use disorder and the highest density of alcohol retail stores. The collaboration will help to dig into the biology and genetics that may belie this correlation.
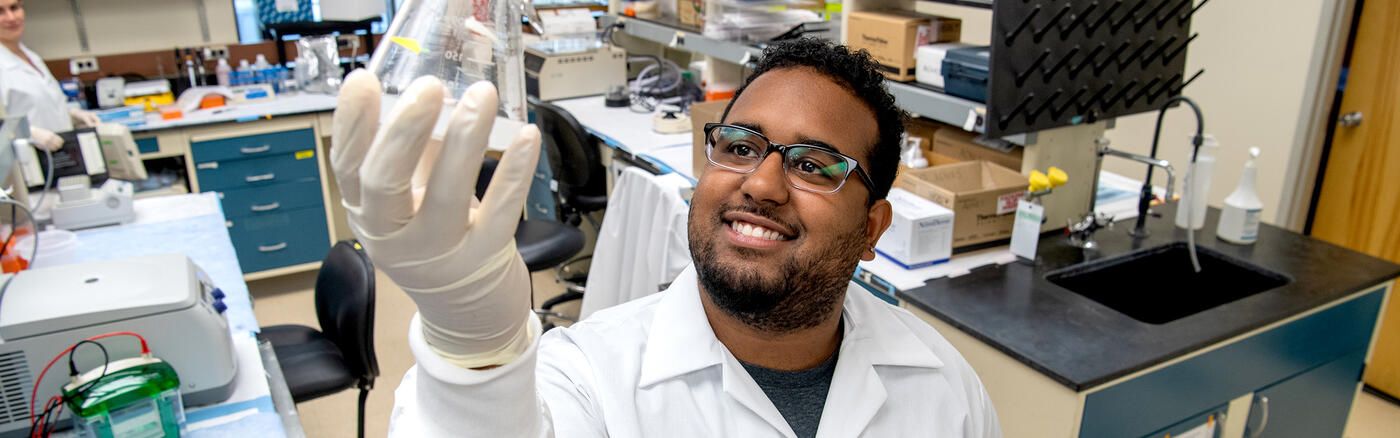
THE RESEARCH PROJECT
The researchers plan to recruit 1,000 women with breast cancer, 500 Black and 500 white. They will biopsy the women’s tumors, which Sims-Mourtada will use to examine differences in gene expression by race. They will also take blood, which Schug will analyze for levels of ethanol and acetate in order to assess the patient’s drinking level, as well as nutrients to get a sense of the patient’s diet. Finally, the researchers will collect extensive patient reported data – including lifestyle, environmental, and socioeconomic factors – which Siegel will assess to determine how the patient’s behaviors and environment relate to what is happening inside their body.
“I think it’s a unique approach to be looking at this multi-level analysis. We’re not just taking into consideration the neighborhood or the behavior, but how those influence what actually happens biologically and genetically,” said Sims-Mourtada.
IMPACTING PATIENTS, PROVIDERS, AND COMMUNITIES
At a patient level, the researchers are hoping to identify biomarkers that would not only indicate risk of developing triple-negative breast cancer but also help detect the cancer sooner than is currently possible via conventional methods.
“Triple-negative breast cancer may start earlier in life before mammography is recommended or develop between screenings. To be able to do a blood test the way one could do a cholesterol test for heart disease, maybe we can see cancer developing sooner,” said Siegel.
The researchers also want to uncover risk factors that healthcare providers can use to educate patients and steer them toward behaviors that match their individual risk level. Alcohol consumption won’t necessarily increase cancer risk for everyone. But it will for some, and those individuals should be informed. With just gentle nudges from a physician, simple changes in alcohol consumption could save lives by reducing the probability of breast cancer in certain high-risk individuals.
At a community level, identifying where rates of risk for triple-negative cancer are highest could mean more targeted outreach. To be able to use public health resources in the areas where they could make the biggest impact could amplify effects on many lives.
A LASTING COLLABORATION
Wistar and ChristianaCare’s joint efforts have repeatedly yielded a two-way benefit: basic scientists learn directly from clinicians about the issues clinicians are seeing at the bedside, and the clinicians learn from the scientists about the challenges scientists face as they are trying
to solve problems in the quest for therapeutic solutions.
“We will be publishing in basic science journals, but we will also be changing how we practice in the cancer center, potentially how we do our community outreach, and possibly prevent loss of life as a result of this research,” said Siegel.
“It really has been a special marriage made in heaven,” said Petrelli, “and I see it continuing for a long time.”
SOURCES
- McCarthy, A. M., Friebel-Klingner, T., Ehsan, S., He, W., Welch, M., Chen, J., Kontos, D., Domchek, S. M., Conant, E. F., Semine, A., Hughes, K., Bardia, A., Lehman, C., & Armstrong, K. (2021). Relationship of established risk factors with breast cancer subtypes. Cancer Medicine, 10(18), 6456–6467. https://doi.org/10.1002/cam4.4158
- Cancer of the Breast (Female) – Cancer Stat Facts. Chart Death Rate per 100,000 Persons by Race/Ethnicity: Female Breast Cancer. (2018). SEER. https://seer.cancer.gov/statfacts/html/breast.html